By: Ritu Ganguli
The rapid rise in vaccine production, especially during pandemics and public health crises, is crucial for preventing the spread of diseases. However, the urgency to meet global demands often compromises sustainability. Key challenges include antimicrobial resistance due to overuse of antibiotics, resource depletion and high emissions during fast-track production for emerging epidemics, and the profit-driven practices of large pharmaceutical companies that prioritize efficiency over environmental accountability.
Background: What are Vaccines?
Vaccines are biological preparations designed to stimulate the immune system to recognize and fight harmful pathogens like viruses and bacteria. They work by introducing a harmless part of the pathogen, such as a weakened or inactivated virus, a protein subunit, or genetic material (mRNA), to train the immune system to respond more effectively during future exposures. Vaccines have been instrumental in controlling and eradicating infectious diseases like smallpox and polio, and they continue to save millions of lives annually.
Big pharmaceutical companies (Big Pharma) are major players in the research, development, manufacturing, and distribution of vaccines. Companies like Pfizer, Moderna, and Johnson & Johnson have impactful innovations in vaccine technology, such as the development of mRNA-based vaccines during the COVID-19 pandemic. While these corporations drive life-saving advancements, they are also subject to scrutiny for their pricing strategies, profit motives, and environmental practices. Their role in vaccine production highlights both the promise and the challenges of balancing public health needs with ethical, economic, and environmental considerations.
The Unsustainable Side of Vaccines
The healthcare market is a massive industry that is anticipated to reach $83.4 billion USD by 2025, and the prescription medicine sector is predicted to reach around $1,562.1 billion by 2026. In this massive industry environmental issues such as pollution in the air, land, temperature changes, antibiotic resistance, and wastes are correlated to health consequences. This creates a toxic cycle as these pollutants contribute to about $800 million annually in the United States alone.
Around 85% of the waste produced by healthcare activities is non-hazardous, while the other remaining 15% is hazardous material that includes infections, chemicals, or radioactive waste. Although in low income areas hazardous and nonhazardous waste is not separated, leading to the greater accumulation of hazardous waste. This includes the production of syringes, vials, and packaging materials.
The pharmaceutical industry is also a major contributor to carbon dioxide and methane. The production, transportation, and storage is also heavily energy intensive. Vaccines must also be stored in cold storage units, which consume significant energy for ultra-low temperature storage, while dry ice is commonly used for transportation. The transportation of vaccines relies on air or road freight, which consumes diesel or gasoline. Plastic packaging for medications is another environmental concern as plastics take hundreds of years to decompose. The pharmaceutical industry is estimated to generate about 300 million tons of plastic waste, which is 50% used for single use applications.
Emerging Epidemics: COVID-19’s Impact on Global Emissions
Vaccine manufacturing at a rapid pace is shown through the recent pandemic of the coronavirus. The rapid need for vaccines during the COVID-19 pandemic has impacted global emissions.
Figure 1: Vaccine Use During Pandemics
Figure 2: Daily Vaccine Production and Carbon Emissions
The COVID-19 pandemic marked a period of unprecedented vaccine production. As the pandemic progressed, the demand for vaccines surged, leading to an overwhelming increase in production. During such crises, the sudden, massive demand for vaccines often depletes resources quickly. Figure 1 illustrates the monthly increase in vaccine production during COVID-19, highlighting a dramatic rise from the beginning to the end of the year. Similarly, Figure 2 depicts the relationship between global CO₂ emissions and daily vaccinations, showing that periods of high vaccination demand correlate with spikes in carbon emissions.
While vaccinations are essential for public health, it is crucial to consider their environmental impacts and explore ways to mitigate them. The high production levels during pandemics emphasize the importance of addressing issues such as waste management, energy efficiency in manufacturing, and the adoption of renewable energy sources to reduce the environmental footprint of vaccine production.
Put into Perspective: The Influenza’s Vaccines Impact on Sustainability
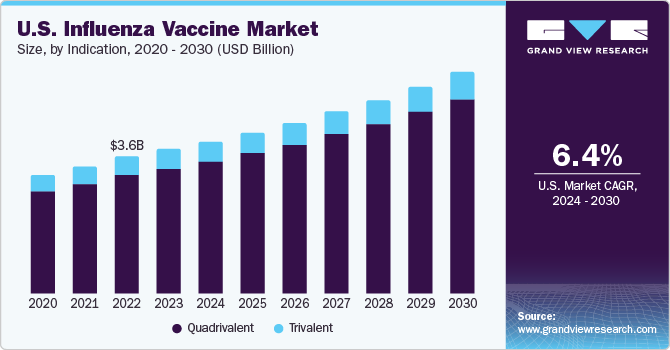
Figure 3: United States Influenza Vaccine Use (2020-2030)
A common sustainability challenge arises from the annual production cycle required for the influenza vaccine. With efficacy rates ranging from 30-60% and only about 30% of the U.S. population getting vaccinated annually, achieving herd immunity remains a significant hurdle. Additionally, traditional egg-based vaccine production necessitates massive chicken farms, consuming substantial resources and generating greenhouse gas emissions. These resources include land and water for large-scale chicken farming, vast quantities of grain to nourish the chickens, energy to maintain farm operations, and transportation to deliver eggs from farms to vaccine manufacturing facilities. Furthermore, the manufacturing process—encompassing cold chain storage and distribution—contributes to a substantial carbon footprint.
The production of the influenza vaccine also generates considerable waste, including plastic waste from syringes, vials, and packaging, biological waste from manufacturing, and chemical waste from production and quality control processes. Because this vaccine is needed annually, its production and distribution maintain a consistent environmental impact year after year. As shown in Figure 3, the demand for this vaccine is increasing over time, necessitating greater production and exacerbating its environmental effects.
While new FDA-approved alternatives to egg-based manufacturing aim to address some of these challenges, they still require annual revaccination and have not fully resolved sustainability concerns. These alternatives strive to eliminate dependence on animal products, provide broader and potentially lifetime protection against multiple flu strains, and reduce the need for yearly production and distribution.
The World Health Organization’s (WHO) Global Action Plan for Influenza Vaccines (GAP) seeks to improve sustainability by increasing seasonal vaccine coverage, strengthening national regulatory frameworks, and promoting local vaccine production in developing countries. Additional strategies to enhance sustainability include optimizing supply management to minimize vaccine waste, using reduced and more sustainable packaging materials, and streamlining packaging to decrease transportation and refrigeration needs.
Vaccine Manufacturing and Antimicrobial Resistance
Antimicrobial resistance (AMR) is when microorganisms such as bacteria, viruses, fungi and parasites no longer respond to antimalarial medicines. AMR is a global threat as it can make infections difficult and even impossible to treat. The release of antibiotics into the environment can speed up the development of antibiotic-resistant pathogens. This resistance could lead to about 10 million deaths annually by 2050. The relationship between vaccine manufacturing and antimicrobial resistance is complex and multifaceted. While vaccines play a crucial role in combating AMR, there are aspects of vaccine production and use that can contribute to sustainability concerns.
Persistent pharmaceutical pollutants in the environment present a complex challenge. Medications like antibiotics, hormones, anti-inflammatory drugs, and chemotherapy agents are formulated to withstand degradation, enabling them to linger in ecosystems well beyond their intended use. Their presence can disrupt wildlife, contaminate natural habitats, and fuel antimicrobial resistance, creating serious threats to environmental health and public safety.
The Lancet takes an unique approach to estimate the amount of deaths that are associated with AMR. They have accumulated data on the number of sepsis-related deaths, the share of infectious deaths linked to specific syndromes, the fraction of syndrome-related deaths caused by particular pathogens, the proportion of pathogens resistant to a targeted antibiotic, and the increased risk of mortality or infection duration due to this resistance. Using these elements, the Landecent calculated the disease burden linked to and caused by antimicrobial resistance (AMR).
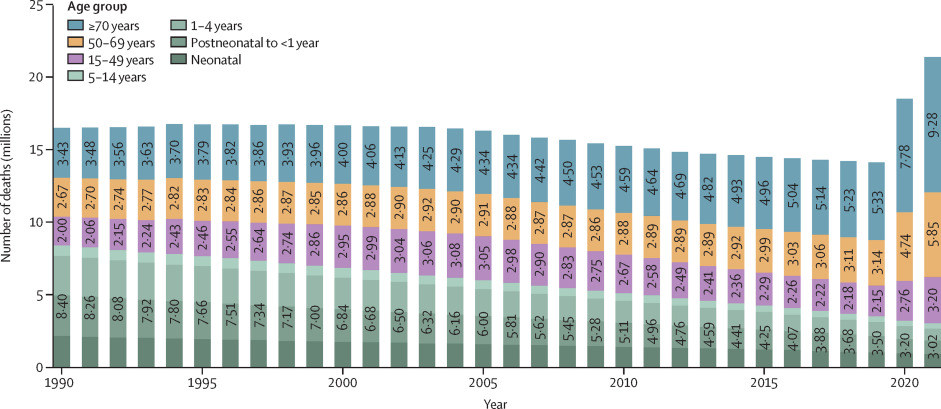
Figure 4: Global time trend of sepsis, by age, 1990 – 2021
Figure 4 estimates the deaths produced by AMR by calculating the global sepsis deaths by age. Overall, the data shows that the total deaths have remained stable until 2019, where it shows a sharp increase. This trend demonstrates that AMR is becoming an increasingly serious global health threat, particularly for older populations. The NIH predicts that there will be 1.91 million deaths attributable to AMR by 2050, and this could reach 8.22 million globally by 2050. South Asia and Latin American regions are forecasted to have the highest all age AMR mortality rates by 2050.
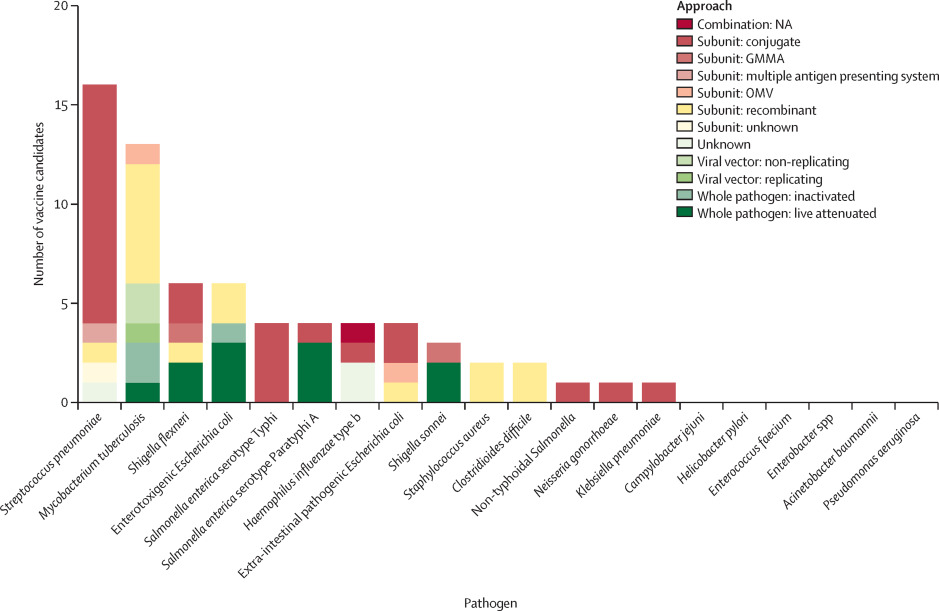
Figure 5: Number of vaccine candidates in active clinical development by approach
Vaccines are highly effective in countering the effects that can occur through AMR. The vaccine candidates in Figure 5 have used many different mechanisms and appliances. Improving the value of vaccines against AMR pathogens can be achieved through the development of combination vaccines with multiple antigen targets. In some areas of disease combination, vaccines have become developed, as they are meant to target multiple pathogens. The rise in vaccinations is directly linked to the increase in production of vaccines, demonstrating how this issue can lead to more unsustainable vaccine production practices and require more resources and time.
Reducing antibiotic usage can significantly decrease infection rates, resulting in fewer antibiotic prescriptions and ultimately reducing the prevalence of antimicrobial resistance. Long-term disease control measures, such as widespread vaccination, are crucial as vaccines offer sustainable protection against infections. Additionally, minimizing antibiotic use can have a positive environmental impact by decreasing the demand for antibiotic production, thereby lowering associated waste and emissions.
The Impact of Pharmaceutical Companies on Sustainability
Pharmaceutical companies research, develop, manufacture and market drugs and other pharmaceutical products to treat, diagnose, or prevent diseases. These companies are a vital part of health care as they focus on researching, manufacturing, investing, and drug regulation.
Through the intensive need and production of vaccines they have been criticized for also leading to unsustainable resources when it comes to vaccine production. Manufacturing practices such as single use plastics and the use of harmful chemicals and energy can lead to high amounts of pollution.
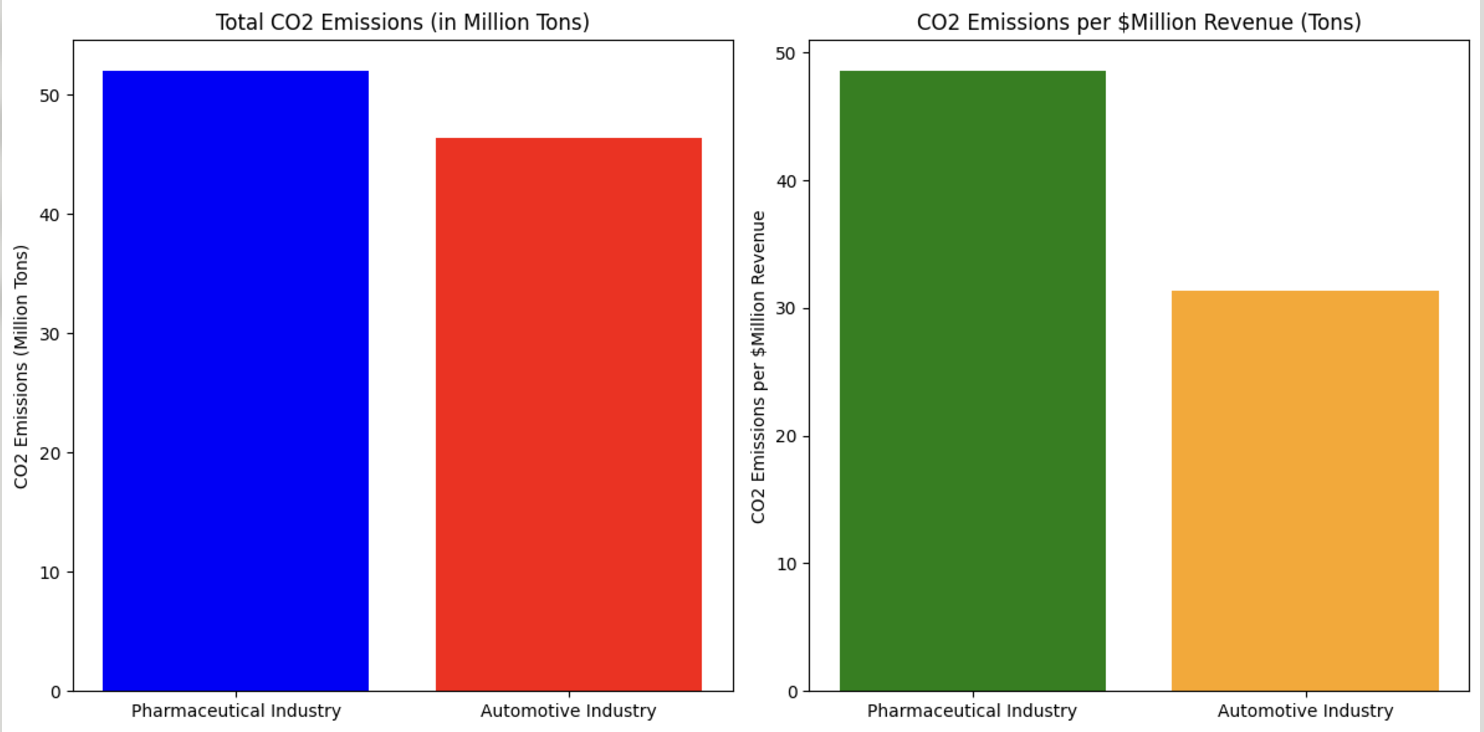
Figure 6 data sourced from The Conversation, graph produced by Ritushree Ganguli
Figure 6: CO2 emissions of the pharmaceutical industry compared to the automotive industry
The pharmaceutical industry is a significant contributor to greenhouse gas emissions, producing approximately 52 megatons of CO₂ annually—a figure equivalent to the emissions generated by 11 million cars in a year. Studies reveal that the environmental impact of the pharmaceutical industry’s pollution emissions is nearly 55% higher than that of car factories and automation. Figure 5 highlights these findings, showing total CO₂ emissions of around 52 million tons annually for pharmaceuticals, compared to approximately 46.4 million tons for the automotive industry. Additionally, CO₂ emissions per million dollars of revenue demonstrate that the pharmaceutical industry emits 48.55 tons of CO₂, whereas the automotive industry emits around 31.4 tons, emphasizing the environmental toll of pharmaceutical production.
Pharmaceutical companies also consume significant amounts of water, often depleting local water resources and introducing harmful pollutants into the environment. Wastewater from manufacturing facilities contains various pharmaceutical pollutants—such as antidepressants, painkillers, antimicrobials, and contraceptives—which have been detected in drinking water, soil, and the food chain, posing risks to both human and environmental health. Additionally, the pharmaceutical industry generates substantial waste, producing approximately 100 kilograms of waste for every 1 kilogram of drug produced. This waste includes: chemical waste, plastic packaging materials, other manufacturing byproducts. Much of this waste ends up in landfills or oceans, contributing to long-term environmental pollution.
Sustainability Initiatives by Pharmaceutical Companies
Many of the largest pharmaceutical companies are taking initiatives towards sustainability.
- Johnson & Johnson aim to use 100% renewable electricity by 2025.
- Novartis: focusing on reducing carbon emissions and water consumption.
- Pfizer: Target at least eight blockbuster cancer drugs by 2030, potentially improving treatment efficiency
- AstraZeneca: one of the first industry to have validates net-zero targets
Despite these efforts, there are challenges that remain within the companies and sustainability measures. Out of 200 companies in the global pharmaceutical market, only 25 of them have reported their direct and indirect greenhouse gas emissions between 2015 and 2019. In the supply chain, it is difficult to track emissions and improve procedures. Plastic packaging within manufacturers is difficult to change. Production is also an energy intensive process that requires very specialized equipment. Additionally, the use of reagents, solvents, and other chemicals used in manufacturing can lead to environmental contamination if it is not well managed.
Systemic Inequalities and Vaccines
Systemic inequalities and power dynamics significantly influence the distribution of vaccines, creating a complex web of challenges that impact global health, economic stability, and sustainability efforts. This inequitable distribution has far-reaching consequences that extend beyond immediate health concerns and hinder progress toward the United Nations Sustainable Development Goals.
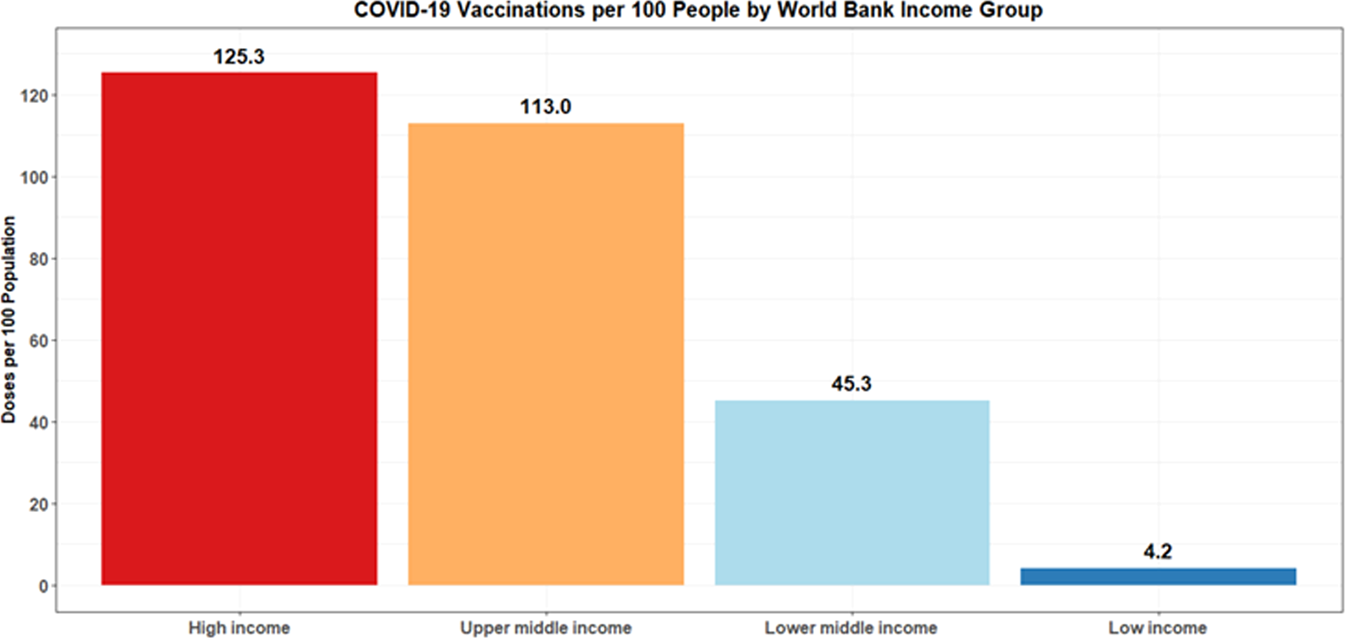
Figure 7: COVID-19 Vaccinations per 100 People by World Bank Income Group
Economic and Political Power Disparities
The distribution of COVID-19 vaccines clearly illustrates how economic and political power shape vaccine access. As shown in Figure 7, for the COVID-19 vaccine high income communities were given much more support with receiving vaccination. High-income countries have been able to secure vaccines through deals with pharmaceutical companies, often at the expense of low and middle-income countries. Countries with greater economic and political power can control vaccine production, trade, and value chains, giving them an advantage in securing doses for their populations. The purchasing power of wealthy nations has allowed them to procure vaccines even before final approval, limiting availability for other countries.This uneven distribution reflects and reinforces existing global inequalities, with poorer nations often left at a disadvantage in accessing life-saving vaccines.
The inequitable distribution of vaccines has several consequences for global health and sustainability efforts. Lower vaccination rates can allow the virus to continue circulating, potentially leading to new variants and prolonging the pandemic globally. This extended health crisis exacerbates economic hardships, pushing more people into poverty and widening the gap between rich and poor nations.
To create a more equitable and sustainable approach to vaccine distribution, several steps are necessary:
- Strengthen Global Health Governance: Improve international cooperation and support for initiatives like COVAX to ensure more equitable vaccine access.
- Invest in Health Systems: Support building robust health infrastructure and systems capable of effectively distributing vaccines.
- Promote Local Production: Support the development of vaccine manufacturing capabilities in low income areas to reduce dependency on global supply chains.
- Incorporate Sustainability in Vaccine Development: Encourage the development of more sustainable vaccine technologies, such as thermostable vaccines that require less cold chain infrastructure.
By addressing these systemic inequalities and power dynamics, the global community can work towards a more equitable and sustainable approach to vaccine distribution. This not only benefits global health but also contributes to broader sustainability goals and helps create a more resilient world in the face of future health crises.
Sustainability Moving Forward
To reduce greenhouse gas emissions and environmental pollutants, several actions can be implemented:
- Green Manufacturing Practices:
- Utilize renewable energy sources to power production facilities.
- Adopt sustainable sourcing of raw materials to minimize environmental impact.
- Effective Waste Management:
- Develop and implement advanced waste management systems.
- Explore alternative methods for disposing of chemical, biological, and plastic waste to reduce landfill and ocean pollution.
- Research and Innovation:
- Invest in research to develop greener manufacturing alternatives, such as plant-based or cell-culture technologies that require fewer resources.
- Transparency and Accountability:
- Pharmaceutical companies can improve sustainability by adhering to established standards and obtaining certifications.
- Increase transparency in emissions reporting and waste management practices.
- Collaborative Efforts:
- Work with regulators, stakeholders, and consumers to align sustainability goals.
- Foster public-private partnerships to promote innovation and shared responsibility in achieving environmental objectives.
A more sustainable approach to vaccine manufacturing not only mitigates environmental impacts but also ensures long-term viability and equitable access to critical healthcare resources. These initiatives can drive meaningful change, reducing the pharmaceutical industry’s carbon footprint while maintaining public health priorities.

No responses yet